An interesting article titled “Prevention of Lingual Nerve Injury in Third Molar Surgery: Literature Review” written by Pippi et al. appears in the 2017 edition of the Journal of Oral and Maxillofacial Surgery (vol. 75, pp. 890-900). The article discusses attempting to identify any factors that could influence if a patient suffers lingual nerve damage after wisdom teeth removal.
In the study the authors reviewed previous literature published up until February 2016 that pertained to lingual nerve injuries after wisdom teeth surgery. From the literature review the authors analyzed three different surgical techniques used for wisdom teeth removal: 1) buccal approach, 2) lingual split technique, and 3) buccal approach plus lingual flap retraction in order to determine if their were any differences on lingual nerve injuries. The authors also evaluated the association between nerve damage and tooth sectioning or ostectomy.
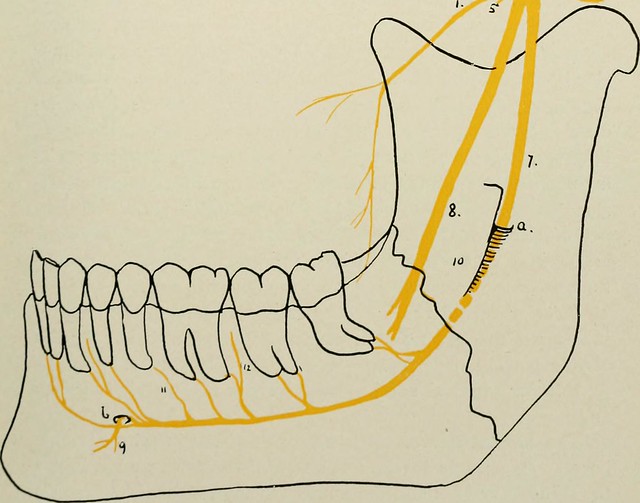
For the lingual nerve in the lower wisdom tooth region the authors included 9 studies in their analysis which showed that average lingual alveolar wall was approximately 3.05 mm and the average vertical distance between the lingual nerve and the top of the alveolar ridge was 7.24 mm. For exploring the surgical technique impact on temporary lingual nerve injury the authors included 28 studies in their analysis and found that the buccal approach plus lingual flap retraction caused more lingual nerve injury than the buccal approach, a result that was statistically significant. For permanent lingual nerve injury there was not any statistically significant difference found between using the buccal approach plus lingual flap retraction or the buccal approach. For exploring the surgical technique impact on temporary lingual nerve injury the authors found the lingual split technique was more significantly associated with nerve injury than the buccal approach plus lingual flap retraction. However, for permanent lingual nerve injury there was not any statistically significant difference found between using the buccal approach plus lingual flap retraction or the lingual split technique. When comparing the buccal approach to the lingual split technique, a statistically significant higher risk of temporary injury of the lingual nerve was found using the lingual split technique but a statistically significant higher risk of permanent injury of the lingual nerve was found using the buccal approach. The authors also determined from 4 articles that tooth sectioning was not associated with permanent lingual nerve damage and that ostectomy was statistically significantly associated with permanent lingual nerve damage.
The authors state
“…although lingual retraction might be associated with a higher incidence of temporary nerve damage, it neither protects nor harms the lingual nerve permanently…Therefore, avoiding lingual flap detachment as much as possible to decrease the incidence of lingual nerve damage is strongly recommended. Lingual nerve protection through the lingual flap should be restricted to selected cases in which the presence of more unfavorable surgical variables predict a high risk of nerve injury.”
Pretty much for all of the results the authors present they say they should be interpreted with extreme caution. This is due to heterogeneity of the data and the influence of anatomic and surgical variables which are difficult to analyze independently. Furthermore most of the studies the authors included in their analysis consisted of studies with small sample sizes. The authors also point out that tooth sectioning could in some cases decrease the extent of ostectomy and aid as a protective factor against lingual nerve injury.
