An interesting article titled “Investigation of nerve injury after lower third molar removal” written by Moosa and Malden appears in the 2018 edition of Oral Surgery (vol. 11, pp. 22-27). The article seeks to address how many patients develop inferior alveolar nerve or lingual nerve injury after wisdom teeth removal at a dental clinic in Edinburgh, UK.
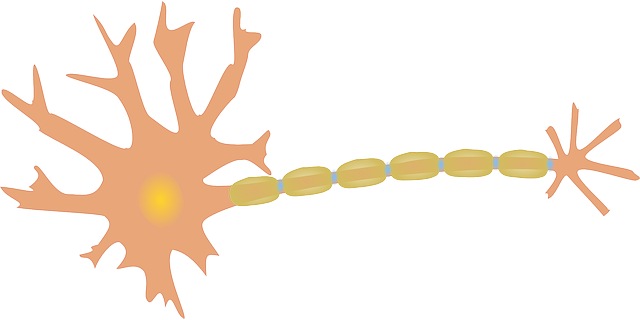
Nerve injury is a type of complication that is known to occur after wisdom teeth removal. Two nerves that are often damaged include the inferior alveolar nerve and the lingual nerve. When the inferior alveolar nerve is injured there can be tingling, numbness, burning, or painful sensations near the lower lip, chin, and teeth. When the lingual nerve is injured there can be tingling, numbness, burning, or painful sensations near the tongue and loss of taste can occur. According to the authors prior studies have tend to shown that permanent inferior alveolar nerve and lingual nerve damage occurs in up to 3.6% of cases and in up to 2.2% of cases respectively. However, these numbers are not always very consistent between study that is conducted.
Therefore the authors sought to conduct a study using 218 patients who had 236 lower wisdom teeth removed at their dental clinic in Edinburgh, UK to determine the incidence of nerve injury. The authors note that in some cases seen at their dental clinic there is a high risk of nerve injury determined to be present after taking a panoramic xray such as by noting diversion of the mandibular canal, darkening of the roots and/or loss of the white lines of the canal. In these cases a cone bone computed tomography scan was conducted to assess the relationship between the nerve canal and the roots of the wisdom tooth. If there was a very close relationship these wisdom teeth were removed using a coronectomy and not included as part of the 218 patients in the study. Based on the panoramic xrays of the 218 patients included in the study the difficulty of the extractions were assessed using the Pederson difficulty index to allow for classification into one of three categories: 1) minimally difficult, 2) moderately difficult or 3) very difficult. All surgeries were performed using local anaesthesia alone or local anaesthesia with intravenous sedation. One week after the surgery each patient received a telephone call where they were asked questions regarding altered sensations in the lip, chin and/or tongue. If they expressed they had altered sensations they were later evaluated at the dental clinic by the use of tests to check for light touch sensation, pin prick sensation, and two point discrimination.
It was found that 67 extractions or 28.4% were classified as minimally difficult, 161 extractions or 68.2% were classified as moderately difficult and eight extractions or 3.4% were classified as very difficult. Only 36 of the extractions were conducted by senior clinicians while the rest (200) were conducted by junior clinicians. Thirteen of the 218 patients had altered sensation when asked over the phone one week after surgery. Eleven of the patients had nerve injury consist with inferior alveolar nerve damage and two patients had nerve injury consist with lingual nerve damage. The authors found the incidence of inferior alveolar nerve injury to be 4.7% and the incidence of lingual nerve injury to be 0.9%. Five of the patients said the altered sensations lasted about a week, six of the patients said the altered sensations lasted about a month, and two of the patients still had altered sensations at the time of publication of the study. The authors did not find any statistically significant differences for nerve injuries when comparing between gender, age, and skill of the surgeon. It was found that 5 extractions classified as minimally difficult resulted in nerve injury, 8 extractions classified as moderately difficult resulted in nerve injury, and no extractions classified as very difficult had nerve injury. The authors state
“When considering the difficulty of the operation, surprisingly, the results contradict most of the available literature. According to the study, as the difficulty of the procedure increased, the incidence of nerve injury not only did not increase but in some of the classifications it decreased as well.”
The authors feel that a study with a large number of patients should be conducted to better assess the risk of nerve injury after wisdom teeth removal. Further it is suggested that there are equal number of cases of each of minimally difficult, moderately difficult or very difficult extractions and that there is an equal distribution of these cases among the surgeons with different skills. Prior studies tend to show that age, difficulty of the surgery, and the skill of the surgeon have an impact on the chances of injury to the inferior alveolar nerve or lingual nerve injury but this was not present in this study perhaps due to poor study design.
