An interesting article titled “Lemierre’s Syndrome Following Extraction of Wisdom Teeth,” appears in the October 20, 2020 edition of the Cureus Journal of Medical Science (written by A. Keshary and M. Hagan, 12(10): e11061). The article describes a case of an 18 year old man who had his wisdom teeth extracted and then developed Lemierre’s Syndrome which rarely occurs after wisdom tooth removal but is is known to affect young and healthy adults; See Near Death Wisdom Teeth Removal Experience where another case has been discussed on this site in the past. Lemierre’s syndrome is a serious bloodstream infection typically caused by Fusobacterium necrophorum. It has a death rate of around 18% and thus if detected needs to be quickly treated with antibiotics. Very few cases of Lemierre’s syndrome after wisdom teeth surgery have occurred since antibiotics became readily available.
In the article, the authors mentioned how the 18 year old man from Kansas developed thrombophlebitis of the veins, specifically thrombosis of his superficial internal jugular vein after his surgery. He did not go to a doctor about this issue until 20 days after having his wisdom teeth removed. Seventeen days after the wisdom teeth surgery he started to experience nausea and vomiting that started with pain and swelling in his left law. When the doctors finally examined him, he was found to have a rapid heartbeat, a low blood pressure reading, his jaw was observed to be swollen and red in color, and an abdominal exam showed he had diffuse lower abdominal and left upper quadrant pain. He was given a CT scan of his mouth, a chest X-ray, and a CT scan of his abdomen. He was started on intravenous antibiotics (vancomycin and piperacillin plus tazobactam) and fluid replacement, and he was admitted to a hospital for evaluation.
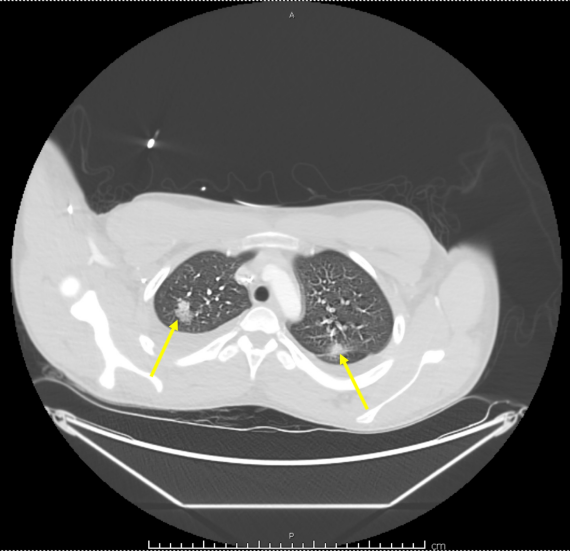
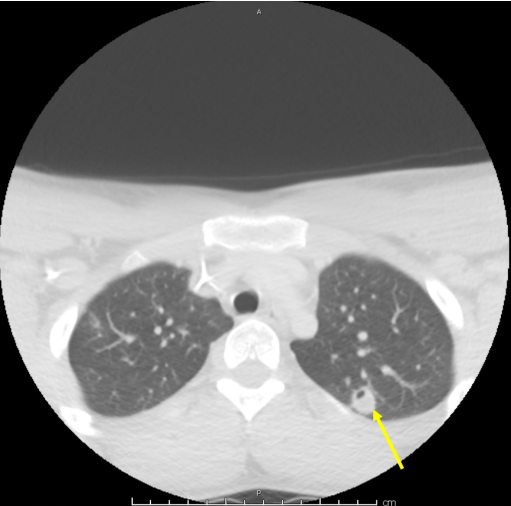
Three days after being hospitalized, he was diagnosed with severe acute hypoxic respiratory failure and was intubated. His condition began to deteriorate rapidly, and he developed septic shock and multiorgan failure. An ultrasound of his neck revealed a thrombosed superficial internal jugular vein consistent with thrombophlebitis, and a repeat chest x-ray showed right lung opacities that indicated pneumonitis. CT angiography (CTA) showed scattered nodular-appearing infiltrates throughout both of his lungs and moderate bilateral effusion. A blood culture was taken and was positive for Fusobacterium necrophorum. A repeat CT scan showed evolving cavitation of the multiple nodular densities seen on the initial chest x-ray that indicated septic pulmonary emboli. A vascular surgeon reviewed the man’s history and suggested that he be managed without any surgery. The man was discharged 12 days after he began to be hospitalized. He had a later follow up CT scan that showed the jaw had a periosteal reaction and was given six weeks of the antibiotic ertapenem. One month after his discharge, additional imaging exams showed that the pulmonary infiltration and superficial internal jugular vein thrombosis had resolved. His left mandibular osteomyelitis had improved but did not fully resolve after one month.
In the article the authors state
“The presence of odontogenic infection with worsening pain and neck swelling should raise high suspicion to obtain necessary blood cultures and imaging for early diagnosis. Given the high mortality rate, emergent imaging is crucial, and there should be no delay in the initiation of antibiotic treatment.”
The authors also mention that diagnosising Lemierre’s syndrome depends on the clinical presentation in conjuction with laboratory results that includes blood cultures
and radiographic imaging exams. A CT scan with contrast can be used to confirm a thrombosed vein such as the internal jugular vein. It is noted that this man’s case is considered atpical as he had thrombosis of a superficial vein. The authors also note that there is no definitive treatment for thrombophlebitis. It is not clear entirely why the authors do not comment on the fact that ultrasound actually made the diagnosis of the thrombophlebitis and it was not found on the initial CT.
