An interesting article titled “A case report on loss of vision secondary to odontogenic orbital cellulitis” appears in Advances in Oral and Maxillofacial Surgery written by A. Ghaesemi and H. Jones (vol. 4, 2021). The article discusses a case of a woman who lost vision after having a tooth extracted.
In the article a discussion is made of a 54 year old woman who went to the hopsital after experiencing three days of left-sided periorbital swelling, nasal discharge, and increasing facial pain. She began to experience these symptoms after having a symptomatic tooth removed. When she arrived at the emergency department she had a left eye that was protruding with extensive conjunctival hyperemia, had restricted eye movements, had a rapid heartbeat, and said that she was increasingly having bluriness in her left eye. A few hours later she lost her ability to see out of her left eye.
A lateral canthotomy was performed and revealed that she had no perception of light in her left eye and increased intraocular pressure. Furthermore, it was found that her left eye had central retinal artery occlusion which is a blockage of blood to the eye’s retina. To help relieve the intraocular pressure, the woman was given an anhloramphenicol ointment, intravenous acetozolemide, an antiobitic, and topical steroid drops.
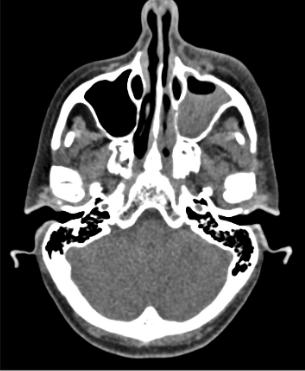
An urgent computed tomography (CT) scan of her sinuses was performed and found that she had a large amount of preseptal and postseptal swelling with retro-orbital fat stranding with small volume fluid noted at lateral and superior left orbit, with no drainable collection in the orbit, which indicated Chandler 2 orbital cellulitis. The can also revelaed partial opacification of the left maxillary sinus and anterior ethmoid air cells. The woman was taken to surgery where was given a lynch Howarth and functional endoscopic sinus surgery procedures. During the sinus surgery, pus was released from her sinus. A culture of the bacteria showed Staphylococcus aureus, a bacterial that can colonize in the oral cavity, which lead to the cellulitis. The woman had eye muscle weakness (ophthalmoplegia) and bulging (proptosis) resolve three days after her sinus surgery. However, even with the surgery and relieve of intraocular pressure the woman’s vision in her left her did not return. An MRI was later performed which showed left superior ophthalmic vein opacification through its length.

The authors say that losing vision from odontogenic cellulitis is rare and does not happen very often. Orbital cellulitis is known to occur from wisdom teeth extraction, although it is not clear which particular tooth the woman had removed in this case. The authors state that when orbitial cellulitis occurs an infection is present and this can lead to increased pressure and bulging eyes. This can consequently cause the compression of the central retinal artery.
The authors state
“Reduction of orbital pressure reduces the degree to which the orbital nerve and ophthalmic artery are stretched allowing for improvement of retinal perfusion…early recognition of [intraocular pressure] rise and its reduction via medical measures may prevent optic nerve ischaemia and central retinal artery occlusion and ultimately preserve vision.”
It is noteworth that the authors note the woman delayed receiving treatment for her problematic tooth for extraction by a dentist and relief of symptoms due to the COVID-19 pandemic.
