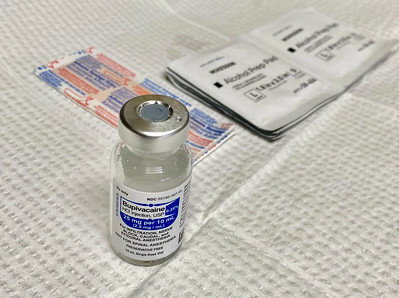
An interesting article titled “A Retrospective Cross-Sectional Study of the Effect of Liposomal Bupivacaine on Postoperative Opioid Prescribing After Third Molar Extraction,” written by Stuart E. Lieblich and et al. appears in the Journal of Oral and Maxillofacial Surgery (vol. 79, pp. 1401-1408, 2021). The study seeks to explore if patients who have lower wisdom teeth removed using liposomal bupivacaine need less opioids than those wo do not have liposomal bupivacaine.
In the study the authors performed a retrospective study of patients who had undergone wisdom teeth extraction at 2 outpatient oral surgery centers in the United States. Patients had to have been at least 18 years of age and undergoing an elective wisdom tooth removal with 1 partial bony or full bony lower impacted wisdom tooth. A total of 600 patients who underwent wisdom teeth extracted were included in the analysis with most of the extractions occuring in 2018 but some occuring in 2012. Data from 2013 and 2017 was not included due to the oral surgery centers changing their pain management protocols. The patients included those who received local infiltration with liposomal bupivacaine (133 mg/10 mL) and patients who did not receive liposomal bupivacaine. A total of 150 patients who received liposomal bupivacaine and 150 patients who did not receive liposomal bupivacaine from each of the 2 oral surgery centers was used. The majority of the patients received intravenous anesthesia for the surgery although a few received a local anesthetic and or nitrous oxide.The 2 oral surgery centers had similar post operative instructions for pain management. One of the oral surgery centers advised patients after surgery to take 600 mg of ibuprofen every 6 hours for at least 48 hours and to first treat any reakthrough pain with 650 mg of acetaminophen 650 mg and if this was insufficient to then use an opioid. The other oral surgery center advised patients after surgery to take 600 mg of ibuprofen and 500 mg of acetaminophen both once daily and if this was insufficient to then use an opioid.
The authors found that those patients who were given liposomal bupivacaine during wisdom teeth surgery were prescribed 59% fewer total opioids versus those who were not. The total amount of prescribed opioids was calculated in morphine milligram equivalents and the rate of prescription refills. After adjusting for age, sex, anesthesia type, American Society of Anesthesiologists physical status classification, and surgical complications, those given liposomal bupivacaine were prescribed significantly fewer total opioids (adjusted MMEs, 44.9 vs 109.5; [95% confidence interval, 0.39–0.44]; P < .0001) and had a significantly lower opioid prescription refill rate (3.3% vs 7.7%; [95% confidence interval, 0.16–0.90]; P = .028) than the group who was not given liposomal bupivacaine.
The complication rate was very similar between groups with 27 patients reporting complications in the liposomal bupivacaine group and 28 patients reporting complications in the group without liposomal bupivacaine. Among those who received liposomal bupivacaine, twelve patients had infections, fourteen had dry sockets and one had nerve injury or numbness versus in the group that did not receive liposomal bupivacaine eight patients had infections, eighteen had dry sockets, and two had nerve damage or numbness. None of the nerve damage was observed to be permanent.
The authors state:
“This study demonstrated that patients who received local [liposomal bupivacaine] LB infiltration received significantly fewer total prescribed [morphine milligram equivalents] MMEs compared with patients who did not receive LB infiltration. A significant reduction was also observed in the proportion of patients requiring opioid prescription refills among patients who received LB, suggesting that the duration of postsurgical pain control with LB may have decreased the need for postsurgical opioids.”
The authors mention some limitations of their study which includes the retrospective nature of the study and the use of electronic medical records which could result in some selection bias. Another issue is a time difference in data from one of the surgical centers. One of the surgical centers had wisdom teeth surgery performed without liposomal bupivacaine in 2012 but the data included in the study with liposomal bupivacaine was from 2018. Due to the 6 year gap in data used, the surgical protocol could have changed as could have patients understanding of opioids. Another issue was that opioid consumption was measured using the number of written opioid prescriptions and refills. Another issue was that the study did not directly compare use of liposomal bupivacaine to another local anesthetic like bupivacaine hydrochloride and thus the opioid-reducing benefits of liposomal bupivacaine compared with local infiltration using other local anesthetics could not be assessed. It is also noted that the use of liposomal bupivacaine does cost additional money and thus has economic implications. Further, it is noted that using more than two oral surgery centers as done in this study would be helpful to reinforce the results and remove potential regional differences. The authors state:
“Further studies including larger sample sizes and different geographical regions, as well as direct comparisons of [liposomal bupivacaine] LB versus other local anesthetics, such as bupivacaine hydrochloride, are warranted.”
The authors feel that adding liposomal bupivacaine during wisdom teeth extractions could significantly reduce the need for opioids use after surgery to control pain. Efforts have been made by dental groups like the American Dental Association and American Association of Oral and Maxillofacial Surgeons to reduce the amount of opioids prescribed as use of opioids for nonmedical opioid use is a problem, see for example the post Dentists Overprescribing Opioids to Adults in the U.S. and Do Oral Surgeons Give Too Many Opioids for Wisdom Teeth Removal?.

Anything to lower opioid use is a good thing.