An interesting article titled “Dental focal infection-induced ventricular and spinal canal
empyema: A case report” appears in the World Journal of Clinical Cases written by Hang Xue an et al. (vol. 8, no. 14, pp. 3114-3121, July 26, 2020). A discussion is made of a case report of a 53 year old woman who developed a brain abscess caused by a dental infection and how an algorithm pathogenic sequencing technique was used for diagnosis.
In the article, the authors discuss the 53 year old woman from China who presented to a hopsital in 2019. She had high blood pressure for 10 years that was not well controlled even though she was taking medication and also had dental cavities for the prior three years. When she arrived at the hospital she was in narcosis and had no autonomous respiration. She had Cerebrospinal fluid (CSF) culture taken to look for any bacteria but did not find any. She had what was called by the authors pathogenic microorganism next-generation sequencing performed to sequence her spinal fluid and evaluate through a compariative analysis against a microorganism database. This sequencing used an intelligent algorithm to indicate that the woman had numerous bacteria typically found in the mouth present in her brain and spinal fluid including: Fusobacterium, Porphyromonas, Solobacterium, Prevotella, Dialister, Fusobacterium nucleatum, Fusobacterium hwasookii, Porphyromonas endodontalis, Solobacterium moorei, Prevotella intermedia, and Dialister pneumosintes.
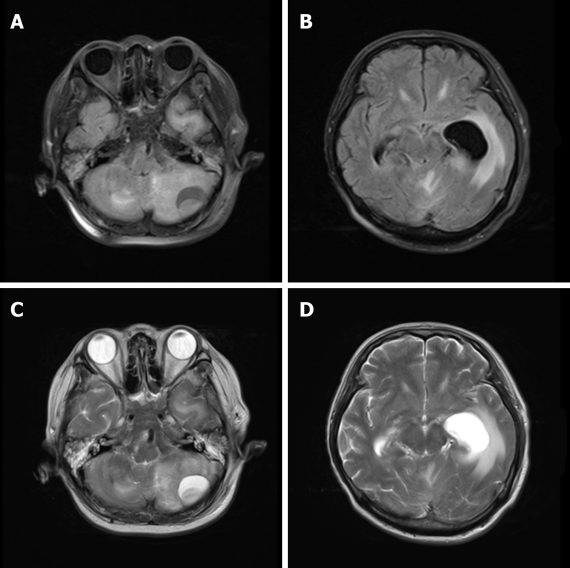
The woman had a brain MRI performed on her head which revealed a quasicircular liquid signal opacity in her left cerebellum. Furthermore, it was found that her adjacent brain stem was compressed, her fourth ventricle became narrower, and ventricular hydrops accompanied by paraventricular edema were present. A spinal MRI was also performed and showed stripe-like long T1 and long T2 signals in C7-T2 spinal canals. She was diagnosed with with ventricular and spinal canal empyema.
empyema: A case report,” World Journal of Clinical Cases written by vol. 8, no. 14, pp. 3114-3121, July 26, 2020 has as Creative Commons license.
As a result of these findings, the woman was given extraventricular drainages and lumbar punctures to treat her ventricular and spinal canal empyema. She was also given antibiotics including meropenem, vancomycin, gentamicin, and S-ornidazole. Unfortunately the woman passed away two months after her initial evaluation at the hospital due to brain stem injury-induced respiratory circulatory failure. The authors feel that the delay in the woman receiving the appropriate antibiotic treatment after presenting to the hopsital led to irreversible damage to her brainstem function and eventually resulted in her dieing.
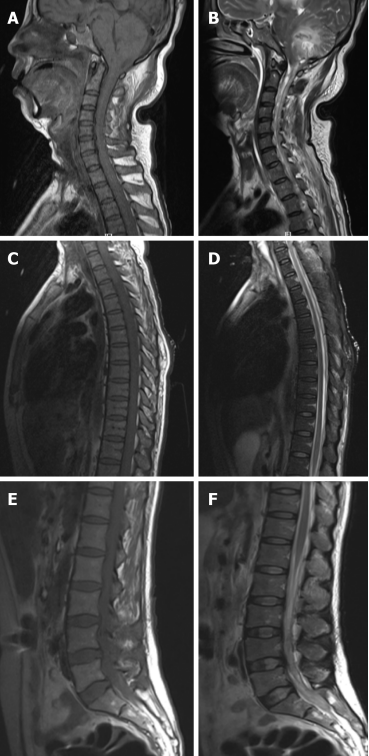
hemisphere and cervical spinal cords, (C) and (D) long stripe T1 and T2 abnormal signals seen in the T1-2 spinal
cord, (E) and (F) flake-like low signal seen in the spinal cord. This image is from Hang Xue an et al. “Dental focal infection-induced ventricular and spinal canal
empyema: A case report,” World Journal of Clinical Cases written by vol. 8, no. 14, pp. 3114-3121, July 26, 2020 has as Creative Commons license.
In the discussion the authors mention that brain abscess is an extremely rare, life-threatening condition, effecting 1 in 100,000 people in the U.S. and when present has a death rate somewhere between 0-24%. Brain abscess that results from the oral cavity is a small percentage of cases and less than 5% of dental focal infection-induced brain abscesses cause pyocephalus which is an outflow of pus in the skull. The authors feel that the woman’s brain abscess was most likely caused by systemic hematogenous infection. They state that dental surgery can cause periodontal vascular endothelial damage which leads to large amounts of oral bacteria entering the bloodstream. They note that in patients with high blood pressur like the 53 year old woman, the blood brain barrier is broken and bacteremia can occur. The authors further note that while CSF bacterial culture is an essential part of medical care, it is not always able to effectively identify pathogens when the source of infection is suspected to be from the oral cavity. The authors state:
“…numerous oral bacteria are fastidious pathogenic bacteria, which may not necessarily grow in culture sufficiently to allow easy identification. Some bacteria induce infection only in the presence of other pathogenic bacteria, and they are called concomitant pathogens.”
It is not clear how widely used the so called next-generation sequencing is that was performed in this woman’s case. Since traditional bacteria cultures can not always detect bacteria from a dental origin it would seem that employing next-generation sequencing in cases like this can be the difference between life and death.
